Maybe there is little new to say about the ongoing opioid crisis, and yet the crisis continues. Perhaps it is time to admit that we may have disregarded something, left an element unexamined.
If we have overlooked anything, it is not whom to hold accountable. Prescribers, distributors, dealers, Sacklers, Purdue, Mallinckrodt, the FDA, the DEA—we have seen proven in court and read in newspapers and blockbuster nonfiction books that all the major players knew what prescription opioids could do or had access to the knowledge but willfully ignored it as they watched the crisis play out.
Some are being fined in the millions, or more. Major manufacturers of oxycodone—the disaster’s primary driver—made billions releasing the generic and the name-brand version of the drug, OxyContin, in quantities that could only lead to widespread abuse, dependency, and addictionin the 1990s and early 2000s. Many, however, are dodging responsibility and declaring bankruptcy to avoid paying government-imposed fines; even those who do pay admit to no wrongdoing.
The search for accountability has done nothing to mitigate the impact of the crisis. More than a million Americans have lost their lives to drug overdose since OxyContin’s release in 1996. That the crisis has endured for so long is devastating; worse is that so many knew oxycodone to be habit-forming back in the 1970s. And in the 1950s. Even earlier. In fact, not too long after chemists Martin Freund and Edmund Speyer invented the drug in Germany more than a century ago, there were early glimpses of the havoc their creation might wreak.
Scrutinizing what is known of oxycodone’s development sheds new light on the ongoing opioid crisis. For perhaps what has been overlooked in the race for accountability is how, from its very beginning, the pharmaceutical industry as a whole allowed for and profited from such crises. If our ongoing opioid crisis is merely a byproduct of this essential aspect of modern Western medicine, it’s going to take more than a few lawsuits to end it.
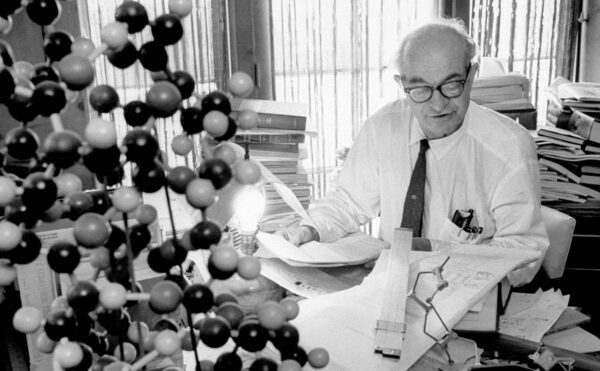
Martin Freund, 1863–1914
Martin Freund’s life in chemistry began at the Realgymnasium in Breslau, then German state Prussia, now Poland. There students trained for careers in the sciences in the secondary school’s well-equipped chemical laboratory. Freund, the charismatic leader of his schoolyard friend group, made ample use of it when he wasn’t reading or hiking.
Upon graduation, his father, ill, induced him to enter the world of business to help feed his five siblings, but it seems that young Martin was not cut out for such work. Freund’s time in a merchant’s office ended in a “dramatic scene in which an inkwell thrown by Martin, or at least raised to throw by Martin, played a significant role,” notes his obituary writer and former schoolmate, L. Spiegel—likely Leopold Spiegel, a chemist at Humboldt University in Berlin.
Did Freund have a temper? Spiegel does not say, only that Freund recommitted to studying chemistry with his father’s blessing but little financial support and with his family’s financial well-being weighing on his shoulders. Does a family’s wealth, or lack of it, affect the kinds of questions scientists ask and guide the projects they pursue? Of course it does.

Freund’s main thing was alkaloids, a potentially lucrative research area with many applications in the still-emerging pharmaceutical industry. So when the well-liked lad graduated from university, he was offered plentiful opportunities for advancement, soon becoming head of the chemistry department at Humboldt University’s Pharmacological Institute.
In 1895 he accepted a lectureship at Frankfurt’s Physikalischer Verein, a demotion of sorts, particularly since the semi-private institute lacked fancy amenities. But the Physikalischer Verein was prestigious enough to attract rich benefactors, which appealed to Freund. Spiegel explains that these benefactors provided whatever was lacking much faster than could be had at a university, where government ministries oversaw all spending. The position in Frankfurt also offered Freund the role of public intellectual, as lectures were open to all comers, not just enrolled students. As a result, his name recognition proliferated over the next decade.
In 1914 World War I began. Germany declared war on Russia, somehow by attacking France. There was excitement in the air, or agitation—a lack of concern for consequences. In Frankfurt a new research university was opening, beholden to neither church nor state, today known as Goethe University. The institution was funded by the city’s prominent Jewish families, including those of entrepreneur Wilhelm Ralph Merton and the German chemist and industrialist Leo Gans.
The rapid spread of World War I meant injuries were occurring at an unprecedented scale—which, if one squints a bit, can be seen as a business opportunity.
“Freund enthusiastically supported the efforts to establish a university in Frankfurt and welcomed the realization of this project with particular joy,” Spiegel tells us. But the new venture was untested. Lack of religious or government oversight meant private interests—like those Freund was growing to favor—could hold sway over his academic research.
The new university absorbed the Physikalischer Verein and inherited Freund, who was made a full professor and director of the school’s chemical institute. Inside the lab, Freund worked to further clarify the compositions of narcotine, morphine, and codeine—the three opium alkaloids that held the most promise for pharmaceutical use. Outside the lab, Spiegel tells us, Freund established close ties to industry. According to researcher Carsten Burhop, Freund had become one of the first academics to formalize a research affiliation with pharmaceutical company Merck back in his Humboldt University days. Throughout his career, the chemist maintained relationships with Cassella, a pharmaceutical and chemical company formerly owned by Gans, and the chemistry arm of Metallgesellschaft, a multifaceted conglomerate owned by Merton.
The rapid spread of World War I meant injuries were occurring at an unprecedented scale—which, if one squints a bit, can be seen as a business opportunity. The new university’s affiliation with neither church nor state left Freund’s affiliation available to the highest bidder. And once established at this new university, Freund had an assistantship available. The younger chemist he hired for the position was doing promising work on thebaine, an opium alkaloid that had yet to find commercial application.
Jakob “Edmund” Speyer, 1878–1915
Edmund Speyer graduated from a Frankfurt high school in 1896, then went to Heidelberg to study chemistry. He thanks his parents and brother, Saly, an architect, in his 1901 thesis, Zur Kenntnis der Additionsfähigkeit ungesättigter Verbindungen. Auf Englisch the title is less sexy—On the Knowledge of the Additional Abilities of Unsaturated Compounds—but it earned him a doctorate and qualified him for a prestigious job back home in Frankfurt 13 years later. There, alongside Martin Freund, he would concentrate on thebaine.
It was, it seems clear, Speyer who brought thebaine to Freund, although the man receives no such recognition in Spiegel’s otherwise detailed account of Freund’s life. Speyer is termed a “long-term collaborator” only after Freund is heralded as thebaine’s savior, then not mentioned again in the narrative. (Freund’s wife, Else Lesser Freund, is slighted similarly.)

Unfortunately, Speyer proves more difficult to track through history than his more frequently named collaborator. Fewer public documents testify to his accomplishments; he goes unmentioned in historical texts. What is noted is sometimes incorrect: he is often, for example, credited with Spiegel’s obituary of Freund. Other findings are simply unsubstantiated: he is lauded for advocating the use of vitamin supplements, although no sources are cited. Did Speyer just lose the charisma game, become forgettable in the ravages of time? Or have his accomplishments, by one regime or another, been withheld from public scrutiny?
One thing we don’t know is how the two first met. Perhaps Speyer and Freund became acquainted through Frankfurt’s chemistry or Jewish communities or through Goethe University connections. (Wealthy Speyers helped fund the university, but whether Edmund Speyer’s father, Moses, a merchant, was among them is unclear.)
What we do know is Speyer’s role in the development of oxycodone is a starring one, made possible by his curiosity about thebaine. In 1915 he published Contributions to the Knowledge of Thebaine and Its Derivatives and soon joined the chemistry faculty at Goethe University. Like records testifying to his accomplishments, however, this position would eventually disappear.
In those early days at Goethe University, the future must have seemed bright. There the two worked: Freund, untall (Spiegel assures us) and reedy; and Speyer, wider and more complacent-looking, at least in the photograph on his German Wikipedia page. An unfunny Laurel and Hardy, only in need of studio backing.
Merck, 1668–1914
When Friedrich Jacob Merck purchased the Engel-Apotheke storefront in a town just south of Frankfurt in 1668, pharmacists were drug vendors, shopkeepers offering a good to the public. In 1827, however, the business changed. Heinrich Emanuel Merck, a descendent of Friedrich’s cousin, started manufacturing and selling morphine. The company grew. By 1895, Merck had 714 employees; by 1914, it had 2,082. Its revenues during that period nearly quintupled.
Compared to its competitors, Merck’s R&D team was about one-half to one-third in size; instead the firm contracted with outside researchers to create new products. These chemists were paid annual fees, which were used to help establish labs and hire assistants. Resulting discoveries were owned jointly by Merck and the chemists, and Merck controlled production and sales. A chemist would publish his (for indeed, they were all men) discovery for the scientific community while rights to it were secured and guarded by patents procured in Merck’s name. Profits were shared between Merck and the chemists.
Under German law, a patent had to be used within three years, which incentivized academics to partner with industry, writes pharmaceutical researcher Tobias Cramer. These partnerships saved inventors the “high and necessary costs of product marketing, mostly advertising costs” and offered risk-free compensation in the form of profit-sharing. It was a good deal: chemists were paid if inventions sold but lost nothing if they failed.
Yet such relationships are not always mutualistic. One party tends to benefit more, sometimes at the expense of the other. “While a professor might find it lucrative to cooperate with a firm, he would have had to sign research agreements that limited his academic freedom,” Burhop notes. In most cases these agreements would incentivize labs to take on projects that aligned with the firm’s financial interests; this might keep inventors tied to projects initiated in the experimentation phase that were revealed in development to have potentially damaging consequences.
Crude opium, among its many other accomplishments, is responsible for the alkalyzing craze of the 19th century and, thus, much of modern medicine.
Martin Freund was fine with the arrangement. He had signed a contract with Merck in 1891, taking home the modern equivalent of about $16,000 as an annual retaining fee, although the real money was in developing a successful product. Freund’s first hit for the company was 1897’s Stypticin, an antihemorrhagic drug and the emerging pharma giant’s top-selling product until 1913. During those initial 16 years, Stypticin earned a profit of 1.2 million marks, of which Freund received 31%. In contemporary U.S. dollars, this would be equivalent to $9.4 million, with Freund receiving about $2.9 million, on top of similar contracts he may have held with other companies. Needless to say, this sum would have dwarfed his university paycheck.
Freund guarded his profits carefully. When in 1906 Merck proposed switching to a compensation model in which Freund would be paid in marks per kilo of Stypticin shipped instead of sharing in profits, Freund calculated potential losses of about five marks per kilo and declined. Freund’s returns dropped anyway, so in a meeting with the company the following year he suggested they revisit the output-based compensation model previously suggested. This time, Merck declined.
Whether Freund hired Speyer because he was promising or because his research was potentially lucrative is unknown. Nor is it known whether Freund paid Speyer with Merck’s marks. We know only that the charismatic chemist brought Speyer’s potentially lucrative research on thebaine to Goethe University just as Stypticin was slipping from its number-one-selling spot.
Thebaine, 1915–1917
Crude opium, among its many other accomplishments, is responsible for the alkalyzing craze of the 19th century and, thus, much of modern medicine. The first alkaloid isolated, around 1804 by German chemist Friedrich Wilhelm Sertürner, was named morphine after the Greek god of dreams, Morpheus. The term alkaloid would be introduced in 1818, and Merck would follow with the commercial manufacture of morphine in 1827.
It was the first modern drug. Thereafter, pharmacists became patent-holders of products they also sold, and the resulting expansion of profitability brought about the modern pharmaceutical industry. (Codeine, another alkaloid of opium, was isolated only a few years after Sertürner’s discovery and made commercially available by Merck in 1836.)
Still, even after the invention of the hypodermic needle in the 1850s, Western medicine continued to rely on crude opium over alkaloid-based drugs. Opium was, researcher Nathan Eddy writes, “the panacea for all ills. When a person became tolerant to its action and dependent upon it . . . more was taken for the aches and pains and other discomforts of abstinence, just as it was taken for similar symptoms from any other cause.” Only at the end of the 19th century did medicine come around to widespread adoption of patented derivatives with Bayer’s release of diacetylmorphine, or heroin, in 1898. In general, these derivatives, now called opioids, were cast, however aspirationally, as “less addicting,” although what they were less addicting than—pure opium?—was not always clear.
If early thebaine researchers shared those aspirations, it appears that they initially were disappointed. Many in the scientific community considered thebaine largely useless, at least in terms of the analgesic and euphoric effects that make opium alkaloids morphine and codeine so popular. Worse, thebaine derivatives could cause spasming and even heart damage.
Spiegel explains that Freund and Speyer’s work on thebaine was intended to distinguish it from morphine and codeine. But were Freund and Speyer hoping to prove or disprove that thebaine, morphine, and codeine could all produce similar results? Prove, it seems. Freund and Speyer “succeeded in converting thebaine directly into codeine,” Spiegel writes. The similarities between the three alkaloids—and thus the commercial potential of thebaine—could no longer be denied.
When Eukodal hit Europe, intelligent people may have believed themselves protected from addiction by, essentially, privilege.
Yet turning a useless alkaloid into a commercial one was only the beginning. “The transition of thebaine to oxycodeinone,” Spiegel explains, “is even simpler; when appropriately reduced, this oxycodeinone yields a dihydro product, the chlorine hydrate of which unexpectedly turned out to be an extremely effective narcotic (‘Eukodal’).”
Freund and Speyer describe the process of creating and naming the new drug in a 1916 issue of the Journal für Praktische Chemie. The publication date marks Merck’s involvement and signals Speyer’s formal affiliation with the company. The new substance “differs in composition from codeinone only in the additional content of one oxygen atom,” the chemists write. “We therefore propose the new oxidation product hydroxycodeinone or oxycodeinone for short.”
The even shorter term oxycodone seems to have emerged later in the United States, shortened again to oxy some 75 years after the drug’s invention. Little more than a bit of trivia, perhaps, but these ever-shifting names have helped obscure the fact that the drug has circulated in the United States for close to a century.
Eukodal, 1917–1929
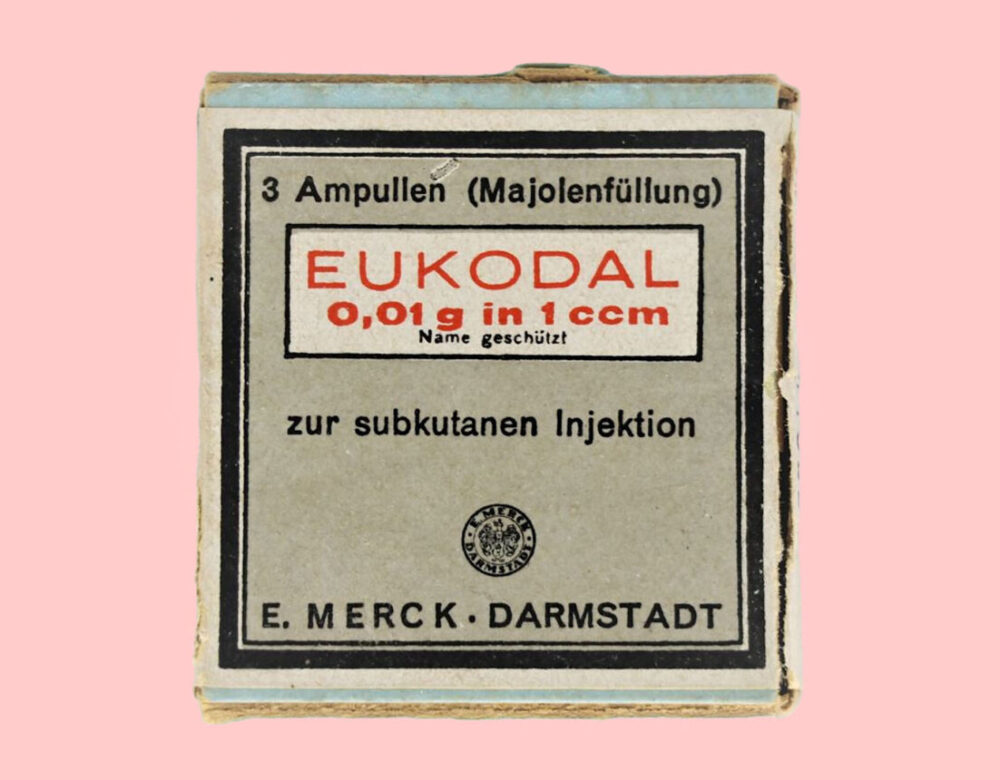
Merck began producing oxycodone commercially under the brand name Eukodal in 1917. Painkillers do well during wartime. Eukodal was an immediate success.
The new drug seemed to offer improvements over other available analgesics. “It is a narcotic like codeine and morphine, but not only works much faster than codeine, but even surpasses morphine,” writes Alfred Schneider in his 1917 compendium of German pharmaceuticals. It also seemed to resolve problems with tremors and heart damage previously associated with thebaine.
When Germany surrendered at the end of 1918, plenty of soldiers went home with Eukodal. Marketed to the public as an effective pain reliever and cough suppressant, by 1920 it was available throughout Europe in ampules or handy pill tubes with metal caps. Each pill contained 5 milligrams of oxycodone, with a suggested dosage of one-half to a full tablet up to three times per day—a lower dose than the Mayo Clinic recommends for severe pain today, of 5 to 15 milligrams every four to six hours. Packaging describes a “sedative and anodyne medicine that calms the irritation of the cough and is used successfully in all diseases of the respiratory tract, as well as in all painful states.” No secondary effects or contraindications are listed.
Notions of drug addiction were still evolving in 1920: was dependency a chemical problem or a human one? Was it contained within a substance, physical defect, moral flaw, or learning disorder? This is still under debate, but uncertainty about the nature of addiction only offers partial explanation for why a drug now understood to house serious abuse potential came with no initial warnings of danger.

To some degree, opium addiction was considered a Chinese problem. The Opium Wars, which the British fought to distribute the drug in China and the Chinese fought to curb its import, were a little more than 50 years in the past, and opium dens still tended to be located in Asian neighborhoods in Europe and the United States.
As David Herzberg points out in White Market Drugs, theories of addiction are always set within pre-existing ideas about race, class, and gender. So even if the copywriting team on Merck’s Eukodal account had understood that the drug was remarkably similar to the one to which mass numbers of Chinese citizens had become addicted, it may have concluded that addiction is a flaw inherent to a race of people; that it was a moral failing that could be eradicated by certain forms of government; or that it could be undone by proper Western education. When Eukodal hit Europe, therefore, intelligent people may have believed themselves protected from addiction by, essentially, privilege.
Yet by 1924 Eukodal had “already resulted in a number of cases of eukodalism, which is not substantially different from morphinism,” according to minutes from a meeting of the Health Committee of the League of Nations. At the meeting a Professor Knaffl-Lenz urged the committee to apply stricter standards to the spate of emerging opium derivates, including Eukodal, that followed the 1912 passage of the International Opium Convention, the first global drug-control treaty. The committee declined to decide the matter, but its report cites four papers, published as early as 1919, testifying to Eukodal as habit-forming and containing abuse potential.
The U.S. patent for Eukodal went through in 1922, although Merck never ended up distributing it stateside. Even if the drug wasn’t officially available to the flappers and dandies of the Roaring Twenties, it was still available. By the end of the decade, Eukodal—oxycodone—was contributing to a national moral panic.
In 1929 Earl Albert Rowell, organizer for the California White Cross International Anti-Narcotics Society, released a book called Battling the Wolves of Society. This screed against narcotic use among young people—his organization’s tagline was “Save youth from dope”—was inciting national conversation about addiction. Montana’s Billings Gazette devoted two columns to Rowell’s local book event, an allocation of resources that likely reflected city concerns.
Youth, Rowell claimed, were the primary targets of an emerging problem in America, one less about drug availability than about the desire for profit that accompanies consumer culture. Yet the victims of drug-pushing profit-mongers represent all ages, nationalities, professions, and income levels, Rowell found. And this addiction, he suggested, causes criminality—not the other way around.
Rowell’s approach to drug addiction—as a medical problem requiring treatment, not a criminal act demanding incarceration—remains upsettingly controversial.
Most theories of addiction at the time held that only lesser elements of society were prone to it—a loosening of strictly racist beliefs into merely classist ones. Rowell disagreed. “Because of the excessive cost of morphine and its allies, addicts, having used up their income, resort to crookedness,” the Gazette summarizes.
It was also unusual to name profitability as a factor that contributed to addiction. For if the evil inherent in addiction lies not in the drug or the user but solely in the ability to profit from a substance, then the drug seller, the drug purchaser, and the drug user are all victims. Of capitalism.
Yet capitalism was not Rowell’s primary concern. His vendetta was against opioids; he singles out Freund and Speyer’s invention by name. And how were the youth of America getting their hands on Eukodal, some 21 years before any form of oxycodone would be legally available stateside? Likely in much the same ways that people acquire illegal drugs today: through friendly international travelers with prescriptions; factory employees or medium-scale suppliers with factory contacts; larger-scale dealers, yes, eager to make a buck, perhaps because living-wage jobs are not always plentiful; and from medical professionals, many of whom felt and still feel that supplying high-functioning people in addiction with maintenance dosages was and remains a core tenet of the medical obligation to do no harm.
However progressive, Rowell’s approach to drug addiction—as a medical problem requiring treatment, not a criminal act demanding incarceration—remains upsettingly controversial. Certainly his core argument, that rising consumerism leads also to a rise in the consumption of dependency-producing agents, has been almost entirely lost today. It’s unfortunate, considering the central role profitability plays in the oxycodone story.
But the economic upheaval of 1929 would soon drop nuanced global socioeconomic analysis into the toilet. By February of that year, Eukodal was in such high demand in the United States that the British Medical Journal noted its proliferation. “Chemists have recently produced two new compounds—eucodal (derived from thebaine) and dicodid (derived from codein),” the journal notes. “The expert committee of the League of Nations holds that both are habit-forming drugs. Reports from America indicate that they are already well known to the dope vendors in that country.”
The first glimmers of an oxy crisis were coming into view, but Martin Freund never saw them. Freund was 56 when he died on March 13, 1920, of an unspecified illness. “His once steely body,” Spiegel writes poetically, “which he had been used to ruthlessly doing everything with despite some inhibitions that had arisen in previous years, was no longer able to withstand the demands.”
Jakob “Edmund” Speyer, 1933–1943
Edmund Speyer carried on the work he had begun with Freund, although any reactions he may have expressed about eukodalism at home or abroad went unrecorded, were destroyed, or have been lost to time. He must have had some reaction: in response to rising reports of abuse and overdose, Merck added the emetic ipecac powder to the formula in 1927, according to the company.
Speyer never married and appears to have cohabitated with his brother for many years, though even that information comes from a brief, unauthored webpage on Frankfurt’s municipal website. In fact, what has been recorded about the man—and in great detail—is not his purported vitamin advocacy or co-invention of oxycodone, but his manner of death.
A massive purge at Goethe University in 1933 removed Speyer from his academic post alongside 108 other Jewish or otherwise politically objectionable professors—almost a third of the faculty—to no public outcry. “Gentile opposition to the spring 1933 measures in Frankfurt was low,” Jonathan C. Friedman writes in The Lion and the Star. In fact, he adds, “many people considered the laws too lenient.”
The Ahnenpass (Proof of Aryan Ancestry) established a foundation for racially discriminatory legislation, while the 1935 Nuremberg Race Laws stripped Jews in particular of further rights and property. National Socialism declared itself a movement of purity, a program of public health intended to eradicate pathogens from the body politic.
As Norman Ohler writes in Blitzed, “Jews and drugs merged into a single toxic or epidemiological unit that menaced Germany.” Recreational drug use was targeted, as were Jews, described by the Third Reich’s head of the Central Office for Combating Drug Transgressions as major players in the international drug trade. Racist hyperbole—the actual success of Speyer and Freund’s creation on the global black market appears to have gone unnoticed.
The propaganda had a larger aim anyway. Der Giftpilz, a picture book, combined Jews and drugs into a single character, a poisonous mushroom, a message of racial hygiene so clear it was shared in nurseries and grade schools throughout the country. Party drugs were cast as foreign, dealers as greedy, and users as racially inferior degenerates. The messaging corresponded with the Reich’s desire to become an intoxicating force in its own right, to be both addictive and stimulating.
Achieving this effect over a sober nation proved a challenge; by 1940, Milan’s Corriere della Sera reported the widespread use of Pervitin, now known as methamphetamine, among German soldiers and officers. The resulting scandal led to a ban on the drug, but more importantly reminded officers that leadership needed protection from direct association with narcotics.
For years, der Führer’s renowned vitality had been propped up by hormones, steroids, vitamins, and proud vegetarianism, but by 1943 his personal physician, Theodor Morell, was running out of experimental natural substances to inject into him. Morell had developed a healthy side hustle mass-producing the various concoctions he was testing on his primary patient. In late spring the war was taking a turn, and it was hurting Hitler’s tummy. The physician needed to try something new.
Morell had previously expressed concern about the addictive potential of Eukodal, particularly given Hitler’s obsessive tendencies, but there was a big meeting with Mussolini on the books, and the doctor’s job was to get his patient through it. By late spring or summer, Morell administered the first subcutaneous injection of Freund and Speyer’s creation into his patient, noting it faithfully in his records. Hitler’s behavior at the early fall dictator summit was animated and successful, and it aroused suspicion. U.S. investigators assumed he was on Pervitin.
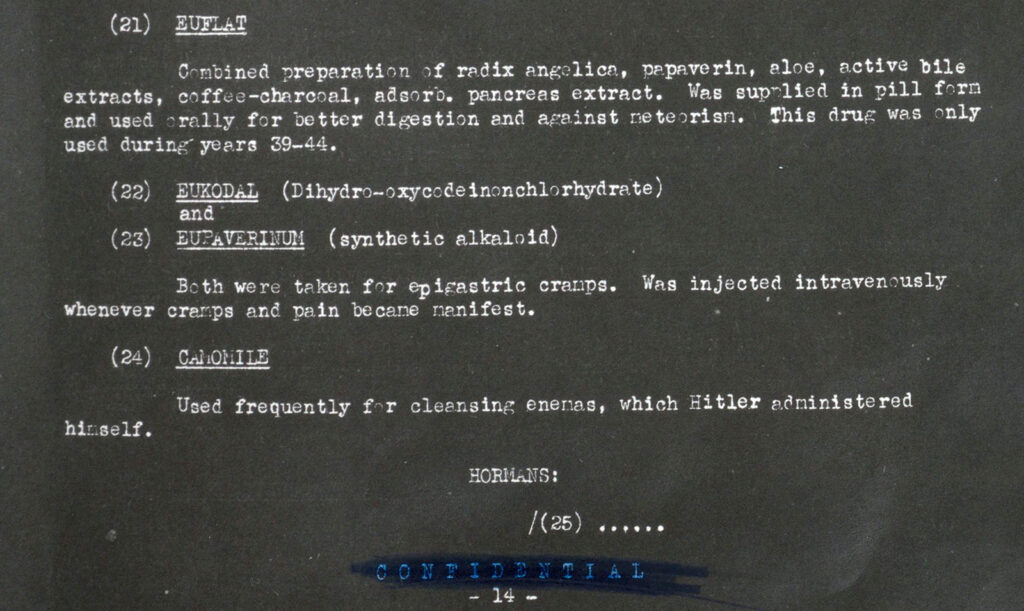
The dictator demanded Eukodal for spasms, flatulence, exhaustion, and anxiety; he also commanded Morell give it to his underlings, including a valet with flu symptoms. Morell began taking injections himself during this time. He does not record what he was using; he only logs complaints when his arm proves difficult to pierce with a syringe. We do know Morell considered Eukodal a success: he began mass-producing opioids himself in the second half of 1943 alongside the experimental remedies he had been testing on his patient.
An attempt on Hitler’s life in July 1944 plunged the patient into pain and anxiety; Morell began a series of unspecified treatments for chronic pain that were likely more Eukodal. The dosage by now had increased: Morell was using 20 milligrams per injection, as often as every other day, Ohler writes. Hitler began exhibiting symptoms of clinical dependency, which Morell noted with concern. But the patient also began acting like an addict. While Reich leadership grew increasingly wary of Morell, Hitler consistently—even violently—defended him. Ohler’s sensationalist text often feels unhinged, but the unadorned facts read like an afterschool special about just saying no.
After a celebratory Eukodal injection on New Year’s Eve 1944, Morell’s records grew sparse as supplies proved difficult to procure in the face of worsening military defeats. Symptoms of withdrawal show up in his notes, as well as symptoms of disease and exhaustion. But had it occurred to Hitler to seek out the creator of his beloved Eukodal before taking his own life on April 30, 1945, it would have been too late.
Truly ending the crisis will necessitate looking at how we define pain, who we believe to be susceptible to it, and what tools we offer to respond to it. No less.
Edmund Speyer had been deported in 1941 to the Łódz ghetto, just 30 miles south of the Chełmno extermination camp, where in December of that year the Reich began gassing Jewish and Romani locals, initiating the Final Solution. Deportations from Łódz began in January 1942. On May 4, Speyer was placed on a train headed north. Marched to an abandoned mill near Chełmno, he spent the night under lock and key without food or water.
The next morning Speyer and an unknown number of others were driven by truck into Chełmno. Remaining valuables and clothes were confiscated. Between 50 and 150 people at a time were marched through a passageway leading to a van lined with sheet metal. When the van was filled, the doors were locked, and gas-masked drivers ran engines until all passengers were dead of asphyxiation.
Speyer’s cause of death was listed as heart failure and exhaustion. The substance he co-created with Martin Freund would be combined with aspirin and released in the United States for the first time by Endo Pharmaceuticals under the name Percodan eight years later, in 1950.
In 2014 a Stolperstein, a Holocaust memorial whose name translates literally as stumbling block, was laid in Edmund Speyer’s honor on the 100th anniversary of Goethe University’s founding, alongside one for his brother Saly, who was also murdered at Chełmno. It is fitting that the institution that supported Freund and Speyer’s collaboration would play a role in Speyer’s commemoration; it is unsurprising that Merck played no similar part, although certainly the pharma giant is responsible for spreading their legacy creation far and wide.
We may never have a complete account of oxycodone’s emergence. It was common for the National Socialists to destroy the records of Jewish scientists; today pharma giants regularly withhold documents pertaining to product development and marketing from public view. Yet Speyer and Freund’s invention continues to have a daily impact on American public health.
Or might we consider it Merck’s product, instead? If we take Rowell’s suggestion, to hold accountable those who profit most from the crisis, Merck should carry the brunt of responsibility here. Yet accountability does little to mitigate ongoing damage. And as we have seen, the opioid crisis is deeply intertwined with the last century of pharmaceutical and social history. Truly ending the crisis will necessitate looking at how we define pain, who we believe to be susceptible to it, and what tools we offer to respond to it. No less.
The year after Speyer’s Stolperstein was laid marked a turning point in the U.S. opioid crisis, as overdose deaths, according to the CDC, surpassed 50,000 annually. Despite a single, hard-earned decrease in overdose deaths in 2018 and 2019, deaths in which oxycodone plays a role continue to rise each year, while newer and more powerful opioids also flood the country.
All translations of German-language sources by the author.