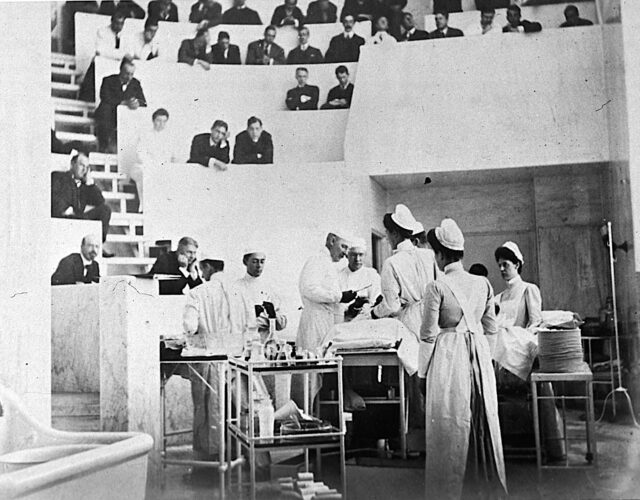
In the age of coronavirus personal protective equipment has become ubiquitous. We all look like surgeons in public now, donning masks and gloves even to go grocery shopping. But however obvious it seems today that protective gear can prevent infections, that hasn’t always been the case. Historically, even simple measures, such as doctors wearing gloves during surgery, were met with fierce resistance.
And while doctors’ lore usually credits a famous surgeon named William Halsted with introducing gloves to the surgical theater, this is a case where the lore is wrong. It wasn’t Halsted who introduced gloves but his now-forgotten assistants. Every time your doctor or nurse, or even a bus driver or grocery clerk, snaps on a pair of gloves, you can say a silent thank-you to Caroline Hampton and Joseph Bloodgood.
Hampton came from a family of South Carolina aristocrats. (Her uncle was Wade Hampton, a famous Confederate lieutenant general.) Sadly, she lost her mother to tuberculosis in 1862, when she was less than a year old, and then lost her father in a Civil War battle a year later. The family fortune suffered a huge blow in 1865 when William Tecumseh Sherman’s forces torched the Hampton plantation. After that disaster the Hamptons were aristocrats in name only, and the orphaned Caroline was raised by three aunts in a tiny home behind the ruins of the old family manor.

The aunts groomed Caroline to be a Southern belle—someone destined to marry a plantation owner. Caroline did take to gardening, although she had to wear gloves to protect her sensitive hands. But the aunts quickly realized Caroline had bigger ambitions than plantation life. She in fact shocked her family in 1885 by announcing she was moving to New York. She wanted to get an education and earn a living for herself by becoming a nurse.
As a nurse Caroline was known for her manual dexterity and her cool, calm demeanor. These qualities made her a natural fit for surgery, and in 1889 she moved to Baltimore and took a job as the chief surgical nurse at the brand-new Johns Hopkins Hospital. Her boss there was William Halsted.
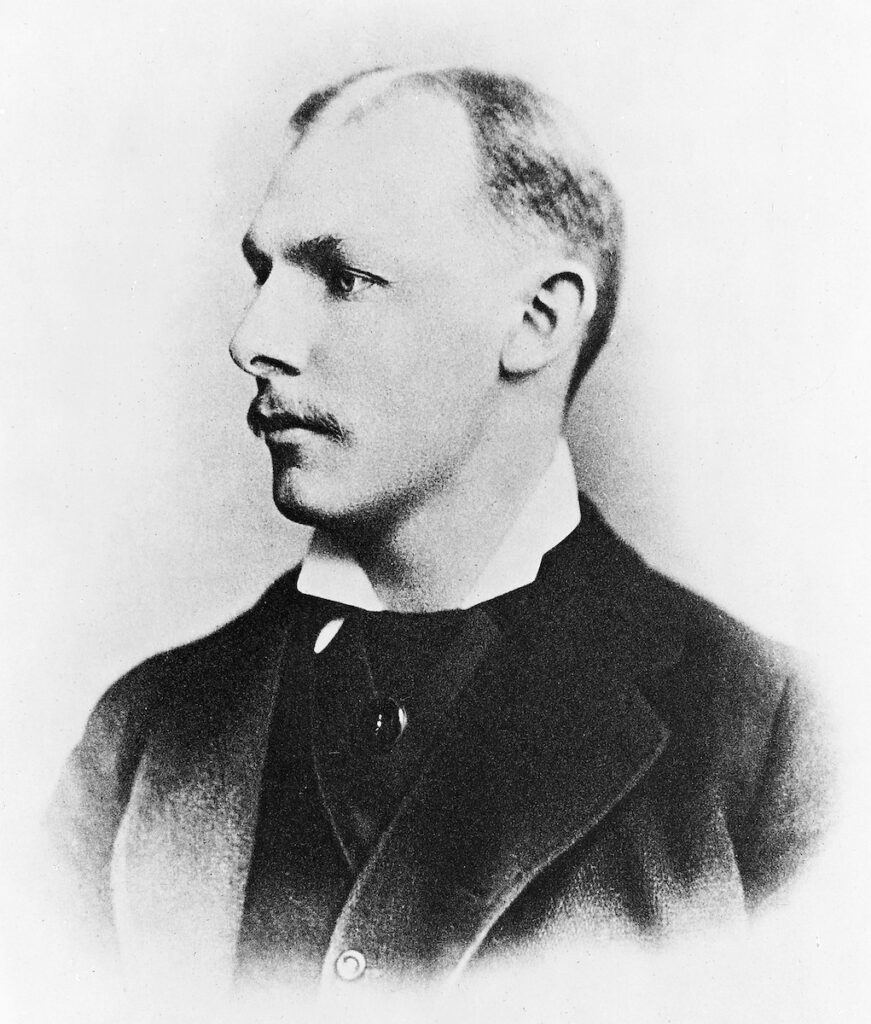
Halsted was regarded as one of the most brilliant surgeons in the country. He’d trained with top doctors in Europe, then settled in New York and developed innovative new procedures for operating on gallstones, thyroid glands, blood vessels, and hernias. He was best known in his day for introducing the radical mastectomy to treat breast cancer—a (now-discredited) procedure where the surgeon excavated not only the tumor but the entire breast and most of the muscles of the chest wall.
One innovation, however, nearly ruined Halsted’s life—cocaine. In the early 1880s he began experimenting with this new drug as a topical anesthetic, notably in eye surgery. It seemed quite promising. To learn more about its effects Halsted, nobly but disastrously, began injecting himself with the drug. He got hooked immediately.
In 1886 Halsted took a six-month leave of absence from his hospital to rehabilitate himself. He missed nine more months in 1887. He finally kicked his dependence on cocaine—but only by replacing it with morphine. The habitual use of morphine was far more socially acceptable in those days but was still a black mark for a doctor. The addiction ruined Halsted’s professional reputation in New York. Only the fledgling Johns Hopkins Hospital would take him on, and even then its administrators placed him on probation from the very beginning.
Halsted kept using morphine in Baltimore but settled into the life of a functional addict. And he did do incredible work at Johns Hopkins, introducing many of the innovations that made the hospital and medical school a legend in American medicine. Many of these improvements involved education; in a rather progressive move for the time, he began teaching Hampton and other nurses the fundamentals of medical science.
Halsted respected Hampton. She was sharp, and he praised her as an “unusually efficient” aide in the operating theater. So he was naturally alarmed in the winter of 1889 when she came to him and announced that she was quitting.
The trouble was her hands. A decade earlier Halsted had enthusiastically adopted the new germ theory of disease and put strict hygienic measures into place. Every person who stepped into his operating theater had to wash their hands with soap, then dip them in a caustic solution of potassium permanganate, followed by a hot oxalic acid bath. And after all that disinfecting they had to wash their hands again with a mercury-chloride compound.
This gauntlet of chemicals certainly killed germs—but also skin cells. Caroline suffered especially badly. She developed severe rashes and eczema, and her skin began peeling. She loved her job, but she couldn’t take the pain anymore.
Halsted suggested she coat her hands in a substance called collodion—a thick, gelatin-like syrup made of nitrocellulose that hardened around her fingers. Unfortunately, the collodion cracked whenever she flexed her fingers, which obviously wouldn’t do.
So they came up with a novel solution: gloves. Back in her plantation days Caroline had worn gardening gloves to shield her sensitive hands. Could suitable gloves protect her here, too?
Halsted paid to get some plaster casts made of Caroline’s hands, then commissioned two pairs of bespoke rubber gloves from the Goodyear Rubber Company of New York.
These weren’t the first gloves ever devised for medicine. A few innovative doctors had used gloves in certain procedures before, especially for childbirth and autopsies. But these earlier gloves were crude things, thick and clumsy and often made of sheep intestines. Worse, they were shaped more like oven mitts than gloves: anything requiring dexterity, such as using a scalpel or sewing up flesh, was out of the question.
Caroline’s gloves, in contrast, were relatively sleek and slender, covering her hands and forearms. They weren’t disposable, of course: people didn’t just throw things away back then. They had to be pulled on over soapy hands and boiled between operations. But they worked brilliantly. Caroline’s hands, safe at last from the acids and mercury baths, healed quickly.
The gloves worked so brilliantly, in fact, that other nurses took it upon themselves to procure their own. Halsted, like many gentleman doctors during that time, was prone to taking long vacations, and he was shocked to return from one such break to see most of his staff wearing rubber gloves, including his male surgical assistants. Caroline had inspired them all. Some of his assistants even reported that the gloves improved their work: they provided better grip for holding instruments than wet, slippery fingers.

So that’s how gloves first entered surgery—to protect doctors and nurses from caustic disinfectants. But within a few years a surgical resident of Halsted’s realized another benefit: gloves also protected patients.
Joseph Bloodgood is the other forgotten pioneer of surgical gloves. With a name like Bloodgood he was probably destined to become a surgeon, and like his mentor Halsted, he did innovative work in several surgical fields, especially cancer treatment.
But the use of gloves in surgery was Bloodgood’s first and most important breakthrough. Starting in 1893 Bloodgood began wearing gloves during hernia operations, and he noticed a drastic decline in postsurgical infections among his patients. In fact the results were so clear-cut they shocked him. Despite all the skin-destroying acids and mercury baths, human hands were still teeming with germs. Bloodgood found that in 220 hernia operations done without gloves, 38 patients went on to develop infections, more than 17%. But in 226 hernia operations done with gloves, only 4 patients got sick—less than 2%. In an era before antibiotics that was an earth-shattering improvement.
Bloodgood published his findings in 1899 and—probably predictably—faced an immediate backlash. Some of the antipathy to gloves was caused by the innate human tendency to resist change. Some was a holdover from the macho days of blood-encrusted coats: surgeons were supposed to embrace gore, to literally soak it in. Gloves seemed soft, a cheat for those who couldn’t hack it.
But some resistance to the use of surgical gloves was more rational. Touch, more than any other physical sense, guided surgeons through operations at that time. Surgeons had to know how different organs and tissues felt inside dark cavities, and they had to know the different textures of diseased and healthy tissue to know which parts to cut.
Rubber gloves, they feared, would numb their fingers and blunt that crucial guide. Detractors argued that any gains from the lower infection rates might be overwhelmed by the hack jobs that would result from touch-blind surgery. One group of doctors even hunted down three blind women and had them read pages of braille while wearing rubber gloves, all to “prove” that gloves obliterated tactile sensation.
However reasonable, this argument turned out to be wrong. The risk for infection was vastly higher than the risk of a surgeon’s clumsiness during an operation. And while gloves did diminish sense of touch somewhat, the introduction of thinner latex gloves soon minimized the problem. In fact, as Halsted’s nurses and assistants found, gloves actually improved dexterity in another way, by providing better grip.
Not every surgeon adapted. Older doctors especially would still strip off their gloves in frustration during ticklish procedures. And there are reports of surgeons who were still fishing around inside people’s guts with their bare hands as late as the 1960s.
For most, though, the benefits of gloves were too obvious to ignore, and by 1911 half of all surgeons were wearing them. The adoption of gloves smoothed the way for other protective equipment, too. Facial masks were being used in half of all operations by 1919.
Halsted later marveled at how stupid he had been in not seeing the hygienic advantages of gloves right away. But to his credit he soon began preaching the virtues of protective equipment to anyone who set foot in Johns Hopkins Hospital. That’s probably why he gets credit today for introducing surgical gloves.
There is one final twist to the story. Giving Caroline gloves allowed Halsted to keep her around for her nursing skills, certainly. But many have speculated that he had an ulterior motive: Halsted was secretly in love with Hampton, and he used the gloves as a way to woo her. Not exactly a dozen roses, but it worked. Hampton and Halsted were married in June 1890—to the chagrin of Caroline’s Southern family, who still wanted her to marry a plantation owner.
While loving overall, the marriage was tinged with some sadness on Caroline’s side. Given the expectations of the times, Caroline resigned her job to marry Halsted and lost her career in the process. It didn’t help that Halsted, while no tyrant, was unbelievably fussy around the house. For instance, he insisted on inspecting every single bean of his coffee. He also insisted on mailing his shirts to Paris to have them laundered because no American firm could meet his standards.
As the one running their household, Caroline had to satisfy all these demands. She began suffering from migraines but continued to enrich her life by reading voraciously and studying French and German. Every year, from April to November, she traveled to North Carolina to run the farm they had purchased there; she also resumed gardening and loved taking buggy rides with her beloved dachshunds, the delightfully named Nip and Tuck. But she spent increasing amounts of time alone, and there’s strong circumstantial evidence that, like her husband, she turned to morphine. And however devoted to each other the couple might have been, one historian observed that the gift of the gloves was about the only tender thing Halsted ever did for her.
Still, that single act brought about one of the most important innovations in medical history. Without Halsted’s gift, protective surgical gear might have been delayed by decades, and millions more people would have died of infections in the meantime.
We’re still reaping the benefits of these innovations today, of course, benefits that have been made all the more obvious during our current pandemic. And for this we can thank a brilliant, drug-addled surgeon who fell for his whip-smart nurse.