William Halford thought he had a surefire vaccine to stop herpes. And he wasn’t going to let anything—laws, ethics, his patients’ well-being—stop him from saving the world.
About The Disappearing Spoon
The Science History Institute has teamed up with New York Times best-selling author Sam Kean to bring a second history of science podcast to our listeners. The Disappearing Spoon tells little-known stories from our scientific past—from the shocking way the smallpox vaccine was transported around the world to why we don’t have a birth control pill for men. These topsy-turvy science tales, some of which have never made it into history books, are surprisingly powerful and insightful.
Credits
Host: Sam Kean
Senior Producer: Mariel Carr
Producer: Rigoberto Hernandez
Audio Engineer: Jonathan Pfeffer
Transcript
The diagnosis hit like a sledgehammer to the face. Cancer. It forever divided William Halford’s world into the blessed, hopeful Before, and the wretched, risky After.
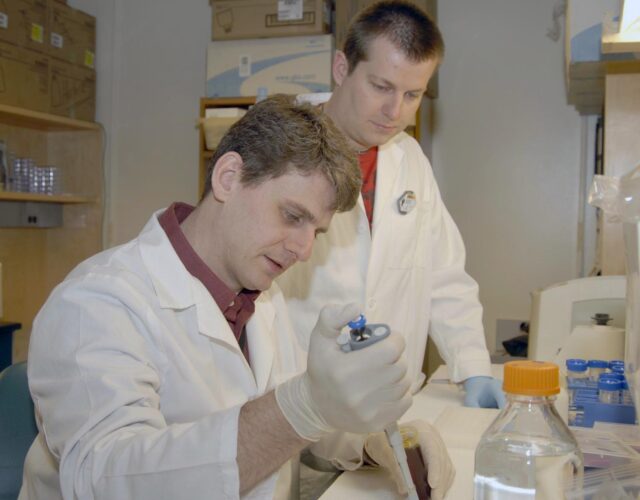
In 2010, Halford was working as a virologist at Southern Illinois University. He looked like stereotypical engineer: square face, square glasses, grey hair. Definitely would’ve worn a pocket protector back in the day.
Halford was a rising star in virology for his work on herpes. In particular, he was developing a herpes vaccine. He hoped it would both prevent people from getting herpes, and lower the severity of outbreaks for those who had it.
Some vaccines use dead viruses, but Halford’s vaccine used a live but weakened form of herpes. Because the virus was alive, he hoped the body would mount a full immune response and learn to fend herpes off. But because the virus was weakened, he hoped it wouldn’t do much damage.
To test his vaccine, Halford gave 160 mice a nasty herpes virus. Some had been vaccinated, some not. Ninety-nine percent of the vaccinated mice lived. Only 6 percent of the unvaccinated mice lived. It was a showstopping result, and he published his results in 2011 to great acclaim.
After that, Halford started putting in 90-hour workweeks to develop the vaccine. He had to. There were so many demands he had to juggle: from colleagues, from vaccine makers, from federal agencies. And even with 90-hour weeks, he was falling behind.
Not surprisingly, he got rundown, and developed a sinus infection he couldn’t shake. So he visited his doctor to get it cleared up, so he could get back to work.
His doctor took some swabs, ran some tests—and returned with grim news. It wasn’t a sinus infection. It was a rare but aggressive type of nasal cancer. Worse, given its location near his brain, doctors couldn’t operate or zap it with radiation. His only hope was chemotherapy and prayers—and it wasn’t clear whether the one would work better than the other.
Halford staggered out of the clinic with his life flipped upside-down. He was 42 years old, with a wife and two kids. He had plans. Cancer didn’t square with any of that.
But cancer it was. And pretty soon, one fear above all gripped Halford’s mind. His vaccine. Could he ever finish it?
The problem, to him, was the FDA, the government agency that controls American vaccines. With all the safety and regulatory hurdles in place, developing a herpes vaccine would take at least a decade—years more than he had.
That’s when William Halford made a decision. If life changed the rules on him, well, he decided he didn’t have to play by the rules anymore.
Nine different types of herpes viruses can infect humans, but doctors focus on two: HSV-1, which mostly causes cold sores, and HSV-2, which mostly causes genital sores. And while some people clutch their pearls and faint upon hearing this, herpes viruses are very common. And frankly, not that big of a deal.
Globally, ⅙ of all people between ages 15 and 49 have HSV-2, the genital one. For HSV-1, that rises to ⅔. And most infected people have no symptoms. The virus just sits in their body, doing nothing.
For this reason, many doctors want to destigmatize herpes. If so many people are infected, and it doesn’t really affect their lives, who cares?
But—people do care. Cite all the numbers you want, but large swaths of the public still get hysterical. Even mild, temporary outbreaks cause deep shame and ruin relationships.
And unfortunately, not all cases are mild. In some people, herpes goes on a rampage. It’s the leading cause of blindness in many countries. It can also infect the brain and destroy people’s memories, causing profound amnesia.
Some unlucky folks also suffer from shooting pains and pus-filled boils on their skin. These outbreaks occur over and over throughout their lives.
Overall, herpes is odd, epidemiologically. Again, it’s extremely common and rarely causes damage. But it carries severe stigma. And in the rare cases where things go bad, it can ruin people’s lives.
That’s why William Halford wanted to develop the first herpes vaccine. And he was committed to going through the long, tough FDA process for winning vaccine approval. The Covid vaccine that doctors produced in 2020 was an exception to the rule, because of the acute nature of the coronavirus pandemic. In less dire cases, producing a vaccine is a slog. It can take over a decade and cost hundreds of millions of dollars. In fact, critics often chastise the FDA for putting such burdens on potentially lifesaving treatments.
In Halford’s case, with his cancer diagnosis, he didn’t have a decade. And it ate at him. He began wearing a chain with a jade gemstone on the end. To him, it was a reminder to never waste a single moment.
It’s not clear when Halford decided to go rogue, but he started recruiting patients early. Halford was not a doctor, but he advised patients on their infections. In fact, he always had a group of fawning patients around him.
Their connection to Halford was emotional. Unfortunately, even many doctors still stigmatize herpes, and their patients didn’t feel they could ask for advice. Or the doctors discounted the pain of people with outbreaks, pooh-poohing their suffering.
Halford never dismissed herpes victims. He was patient and kind and took their pain seriously. People with herpes trusted him.
Halford then took advantage of that trust. He began recruiting nine patients for a top-secret underground vaccine trial.
It began in the summer of 2013. Halford rented a hotel room in Illinois, and the nine patients he’d recruited visited one by one. When they arrived, Halford sat them on the bed, then began mixing vials of fluids together.
Halford was undergoing intense chemotherapy then, and patients remember him looking pale and weak. But the chance to test his vaccine invigorated him. For each patient, he wiped the injection spot on their calf with alcohol. Then he drew a circle with a black marker, and injected the vaccine.
In all nine cases, a huge pustule swelled up on the patients’ calves within a few days. It was red and angry, like a volcano. But it eventually died back down. And to the patients’ delight, their conditions generally improved over the next year. For most, the outbreaks stopped.
Halford was thrilled. He’d given his patients real hope. But to take the next step in his rogue vaccine trial, Halford needed money. He would get it from a most unlikely source. Hollywood.
A Hollywood producer—whose credits included a Martin Sheen movie—happened to hear about William Halford’s research through online research. The producer, frankly, was paranoid about herpes. An old girlfriend had it, and despite having no outbreaks himself, he developed a terror of it, a phobia.
He therefore reached out to Halford in 2015 and flew him to New York for dinner. There, he gave Halford $700,000 to found a company and fund Halford’s research.
With the cash, Halford moved into phase II of his underground vaccine trial. To evade FDA scrutiny, he conducted the trial beyond the reach of the FDA, in St. Kitts in the Caribbean. The $700,000 helped rent a house overlooking a gorgeous turquoise bay. Vervet monkeys chattered in the trees.
Halford’s company flew 20 patients down for three rounds of injections over a few months. Like before, Halford drew a red circle on each patient’s leg and injected the vaccine, after which an ugly welt arose. In fact, while the patients were walking around St. Kitts, enjoying the sites, they’d sometimes spot someone with the same gnarly welt. There would be a moment of shocked recognition—then laughter, as they realized they were in the same boat. Many of the patients bonded over this experience, happy to finally meet someone who understood their plight.
Halford nurtured this sense of community. He hosted dinner parties for patients in St. Kitts, where they feasted and drank beer. Halford’s own suffering also brought him closer to his patients. In St. Kitts, they remembered him looking increasingly grey and weary from the chemotherapy. The tumor also damaged his eyes. He began seeing double and had to stop driving. He eventually lost an eye and had to wear an eyepatch.
But his pain—and the ferocious way he pushed himself—made his patients love him more. They could see the sacrifices he was making for them. A common criticism of medicine nowadays is that it’s too cold, too technocratic. You wait for hours, get five minutes with Dr. So-and-so, and leave with pills or orders for yet another test. It’s inhuman.
In the old days, doctors nurtured body and soul. The brutal efficiency of modern medicine leaves people craving connection. Well, Halford’s vaccine trial nurtured connections. He built a real community.
Unfortunately, that very community was part of what made the trial dangerous.
It’s one thing to long for a family doctor to chat with you and nurture your spirit. But a vaccine trial is a different beast altogether, because of the danger of bias.
To evaluate how well the vaccine worked, Halford had to ask people about the level of pain they were suffering and the overall severity of their outbreaks. Those aren’t objective numerical measurements. Pain especially is subjective.
So if you’re a patient in this trial, and you’re having beers and chumming about with the scientist running it, well, you’re more likely to want to please him. And you do so by giving him the answers he wants to hear—that his vaccine changed your life. It’s human nature. For all its joys, friendship introduces bias. You cannot properly evaluate a vaccine in those circumstances.
Even worse, Halford didn’t design his experiment properly. There was no control group—a cohort of people with herpes who got dummy injections. It’s well known, psychologically, that any care and treatment will make people feel better, even if the treatment is worthless. It’s called the placebo effect. And without a control group, Halford had no way of knowing whether the vaccine was actually doing something or if the mere care and attention from a sympathetic soul—from a friend—was the real benefit.
Halford nevertheless plowed forward. And the initial results from the St. Kitts trial looked promising. Several patients said the injections functionally cured them of herpes. They suffered no more outbreaks, no more pain.
Unfortunately, other people got worse. The first injections provided temporary relief. But then the shooting pain and sores came roaring back. One woman also experienced uncontrollable shaking, and said she felt like she was suddenly a hundred years old—decrepit and weak. Some patients outright refused the third vaccine shot.
Sadly, when these patients told Halford about their suffering, he dismissed their complaints—exactly like their doctors had before. He told them their symptoms couldn’t be related to his super-safe vaccine. They must have picked up another disease in the tropics.
In reality, here’s what likely happened. Again, there are two main types of herpes viruses, HSV-1, and HSV-2. The vaccine contained a weakened form of number 2. But some of Halford’s patients probably had HSV-1. So the vaccine was introducing a new strain of virus into their bodies—bodies that were already sensitive to herpes outbreaks. No wonder they suffered.
Halford eventually submitted a paper about his vaccine trial for publication. In it, he claimed that 17 of the 20 patients were fully cured of herpes. But he ignored the three patients who fared worse. Moreover, his obvious attempts to dodge regulatory and ethical rules horrified the scientists who peer-reviewed the trial.
Stubbornly, Halford kept working on his vaccine until the very end, when his body gave out. One night before bed, in summer 2017, his wife saw him take off the jade necklace he wore to remind himself to never waste a single moment. A few weeks later, he died at age 46.
Shortly afterward, three patients sued Halford’s vaccine company, which survived his death. Doing so was not an easy decision for them. Filing the lawsuit required them to go public with the fact that they have herpes. They’d been trying to hide this their whole lives to avoid the stigma. Their decision to sue outed them. But they felt they had no choice. The trial is still pending.
So what should we take away from the case of William Halford? He argued that government regulations stifle potentially lifesaving treatments. And many scientists would agree. Should developing a new drug or treatment really take hundreds of millions of dollars? You’ll all but ensuring that companies will only pursue treatments that will make them lots of money. It skews their values.
Then again, just because Halford was right about one point doesn’t mean he was right overall. In my book The Icepick Surgeon, I dissected several old cases of rogue medical scientists conducing unethical experiments on people. I also explained how safeguards like FDA oversight and institutional review boards can curb such abuses.
I didn’t know about Halford when I wrote Icepick Surgeon, but he shares several chilling traits with other rogue scientists. Most obvious was his tunnel vision, especially after his cancer diagnosis. From that point forward, very little mattered to Halford beyond his vaccine. His desire to test it overrode everything, even the normal medical instinct to do no harm.
Beyond his tunnel vision, Halford’s ego proved destructive. By all accounts he genuinely wanted to help people with herpes. But instead of rushing forward, he should have simply done all the work he could in the time he had left, then trained others to take over after him. Halford didn’t do that. He insisted that he had to see things through. And while his patients appreciated his nurturing approach, his friendship with them undermined the validity of his trial in the end.
Time will tell whether Halford’s vaccine will benefit the world at large. The company he founded still exists, and is still working on his vaccine—albeit by following FDA rules this time. But even if the vaccine works, Halford ruined lives along the way. I do believe that, on many levels, William Halford was a good person. But even good people need ethics.
At one point in The Icepick Surgeon, I mentioned that, despite all the safeguards of modern research, if someone were truly determined to carry out an unethical experiment, society probably couldn’t stop them. I didn’t mean that as a prophesy, just a provocative line to get people thinking. And I have to say, this is one case where it doesn’t feel good to be right.